Gastroshiza might sound like a complex medical term, but it’s actually a condition that affects many people around the world. This digestive disorder involves the splitting or separation of stomach muscles, which can cause significant discomfort and impact your daily life. Whether you’re experiencing symptoms yourself or trying to understand this condition better, this guide will walk you through everything you need to know about gastroshiza in simple, easy-to-understand language.
What is Gastroshiza?
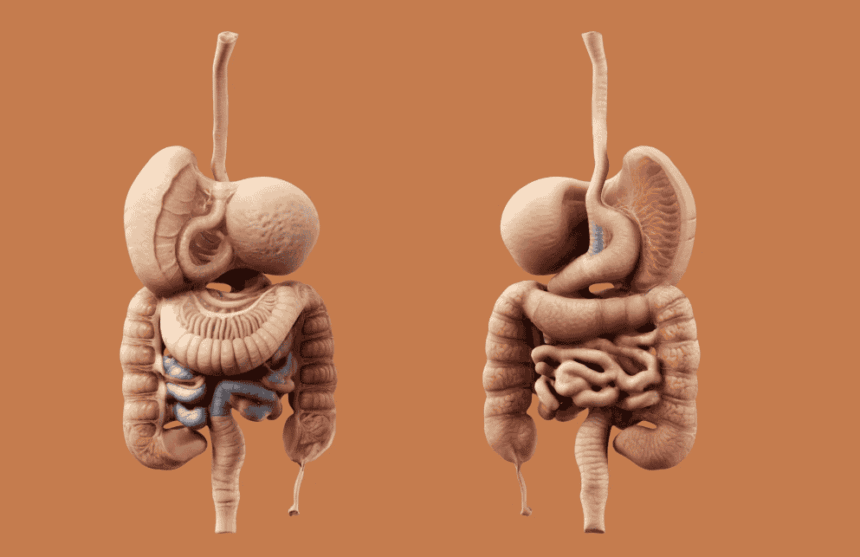
Gastroshiza is a medical condition characterized by the separation or splitting of the stomach muscles, particularly those in the abdominal wall. This condition occurs when the connective tissue between the rectus abdominis muscles (the “six-pack” muscles) stretches and weakens, creating a gap or split. The term comes from Greek origins, where “gastro” refers to the stomach and “shiza” means to split or divide.
This condition is most commonly seen in pregnant women, but it can also affect men, children, and women who have never been pregnant. The separation creates a visible ridge or bulge that runs down the middle of the belly, especially when the abdominal muscles are engaged. Understanding gastroshiza is crucial because it affects not just appearance but also core strength and overall digestive health.
The condition ranges from mild to severe, with some cases requiring medical intervention while others can be managed through conservative treatment methods. According to recent studies featured on TrendsMag, awareness about gastroshiza has increased significantly in recent years, leading to better diagnosis and treatment options for patients worldwide.
Common Causes of Gastroshiza
Understanding what causes gastroshiza helps in both prevention and treatment. The primary cause is excessive pressure on the abdominal muscles, which can occur for several reasons. Pregnancy is the most common cause, affecting up to 60% of pregnant women to some degree. During pregnancy, the growing uterus puts tremendous pressure on the abdominal muscles, causing them to stretch and sometimes separate.
Other significant causes include rapid weight gain, particularly when it involves abdominal fat accumulation. Heavy lifting, especially when done incorrectly or excessively, can also contribute to muscle separation. Genetics play a role too – some people are born with weaker connective tissue that makes them more susceptible to developing gastroshiza.
Age is another factor, as the connective tissue naturally weakens over time, making older adults more prone to this condition. Certain medical conditions, such as chronic coughing or severe constipation that causes repeated straining, can also lead to muscle separation. Understanding these causes helps individuals take preventive measures and seek appropriate treatment when needed.
Recognizing the Symptoms
The symptoms of gastroshiza can vary significantly from person to person, but there are several common signs to watch for. The most obvious symptom is a visible bulge or ridge that appears down the middle of the belly, particularly when sitting up or engaging the abdominal muscles. This bulge becomes more pronounced when coughing, laughing, or straining.
Many people with gastroshiza experience lower back pain due to weakened core muscles that can no longer properly support the spine. This pain often worsens with physical activity or prolonged standing. Digestive issues are also common, including bloating, constipation, and a feeling of heaviness in the abdominal area.
Other symptoms include:
- Difficulty with everyday activities like lifting objects
- Poor posture due to weakened core support
- Pelvic floor dysfunction
- Reduced exercise tolerance
- Feeling of abdominal weakness or instability
Some individuals may also experience psychological effects, including decreased self-confidence due to changes in abdominal appearance. It’s important to note that symptoms can worsen over time if left untreated, making early recognition and intervention crucial for optimal outcomes.
Types and Classifications
Gastroshiza is classified into different types based on location, severity, and characteristics. The most common classification system divides the condition into three main categories: supraumbilical (above the belly button), infraumbilical (below the belly button), and complete separation that extends the entire length of the rectus abdominis muscles.
Supraumbilical gastroshiza typically occurs in the upper abdomen and is often associated with pregnancy or significant weight gain. This type is generally easier to treat and may respond well to conservative management. Infraumbilical separation is less common but can be more challenging to address, often requiring more intensive treatment approaches.
The severity is typically measured in finger widths, with mild cases showing a separation of 1-2 finger widths, moderate cases showing 2-3 finger widths, and severe cases showing more than 3 finger widths. Some medical professionals also classify gastroshiza based on depth, measuring how far the fingers can sink into the separation when examining the patient.
|
Type |
Location |
Typical Width |
Treatment Difficulty |
|---|---|---|---|
|
Supraumbilical |
Above navel |
1-3 finger widths |
Moderate |
|
Infraumbilical |
Below navel |
1-2 finger widths |
High |
|
Complete |
Full length |
Variable |
High |
Diagnosis Methods and Procedures
Diagnosing gastroshiza typically begins with a physical examination by a healthcare professional. The doctor will ask you to lie on your back and lift your head slightly off the ground, which engages the abdominal muscles and makes any separation more visible and palpable. They’ll then use their fingers to measure the width and depth of the separation.
Advanced diagnostic methods include ultrasound imaging, which provides a more precise measurement of the separation and can assess the condition of the connective tissue. CT scans or MRI imaging may be used in complex cases or when surgical intervention is being considered. These imaging techniques can provide detailed information about the surrounding tissues and help plan the most appropriate treatment approach.
Self-assessment techniques can also help identify potential gastroshiza. You can perform a simple test at home by lying on your back, bending your knees, and lifting your head slightly while feeling for a gap between the abdominal muscles. However, professional medical evaluation is always recommended for accurate diagnosis and treatment planning.
Early and accurate diagnosis is crucial because it allows for timely intervention, which can prevent the condition from worsening and improve treatment outcomes. Regular monitoring may be necessary, especially during pregnancy or weight loss programs.
Treatment Options Available
Treatment for gastroshiza varies depending on the severity of the condition and individual patient factors. Conservative treatment is often the first line of approach and includes specific exercises designed to strengthen the deep abdominal muscles and improve core stability. Physical therapy can be particularly beneficial, with therapists providing personalized exercise programs and techniques.
Specialized exercise programs focus on activating the transverse abdominis muscle, which acts like a natural corset around the torso. Breathing exercises, pelvic tilts, and modified planks are commonly prescribed. It’s important to avoid traditional exercises like crunches or sit-ups, which can actually worsen the separation.
For more severe cases, surgical intervention may be necessary. The most common surgical procedure is called abdominoplasty or “tummy tuck,” which involves surgically repairing the separated muscles and removing excess skin. Minimally invasive laparoscopic techniques are also available for certain cases, offering shorter recovery times and reduced scarring.
Non-surgical options include:
- Physical therapy and specialized exercise programs
- Abdominal binding or compression garments
- Proper nutrition to support tissue healing
- Gradual return to normal activities
- Regular monitoring and assessment
Exercise and Physical Therapy
Exercise plays a crucial role in managing gastroshiza, but it must be done correctly to avoid making the condition worse. The key is focusing on exercises that strengthen the deep core muscles without putting excessive pressure on the separated tissues. Working with a qualified physical therapist who understands this condition is highly recommended.
Effective exercises include diaphragmatic breathing, which helps activate the deep core muscles and improve coordination between the diaphragm and pelvic floor. Wall sits, modified planks, and dead bug exercises can help build strength gradually while protecting the healing tissues. Progressive resistance training should be introduced slowly and under professional guidance.
It’s equally important to know which exercises to avoid. Traditional abdominal exercises like crunches, sit-ups, and planks can increase intra-abdominal pressure and worsen the separation. Heavy lifting, especially overhead movements, should be avoided until the condition improves significantly.
Safe Exercise Progressions:
- Beginner Level: Breathing exercises, gentle stretching
- Intermediate Level: Modified planks, wall sits, pelvic tilts
- Advanced Level: Functional movements, progressive resistance training
- Return to Sport: Sport-specific movements with proper form
Consistency is key when it comes to exercise therapy for gastroshiza. Most people see improvement within 6-12 weeks of consistent, proper exercise, though complete healing may take longer depending on the severity of the condition.
Prevention Strategies
Preventing gastroshiza involves maintaining strong core muscles and avoiding activities that put excessive strain on the abdominal wall. For pregnant women, prenatal exercise programs can help maintain core strength and reduce the risk of severe muscle separation. Proper lifting techniques are essential for everyone, emphasizing the use of leg muscles rather than back and abdominal muscles.
Maintaining a healthy weight reduces unnecessary pressure on the abdominal muscles. Gradual weight loss is preferable to rapid changes, which can stress the connective tissues. Good posture throughout the day helps distribute forces evenly across the core muscles and prevents excessive strain on any particular area.
During activities that might increase abdominal pressure, such as coughing or sneezing, engaging the pelvic floor muscles can help protect the abdominal wall. Learning proper breathing techniques during exercise and daily activities can also reduce the risk of developing gastroshiza.
For those already at risk, regular self-monitoring can help detect early signs of muscle separation, allowing for prompt intervention before the condition becomes severe. Education about proper body mechanics and movement patterns is crucial for long-term prevention.
Complications and Risk Factors
If left untreated, gastroshiza can lead to several complications that affect both physical health and quality of life. One of the most common complications is chronic lower back pain, which occurs because weakened abdominal muscles cannot properly support the spine. This can lead to poor posture and increased stress on other muscle groups.
Digestive problems may worsen over time, including increased bloating, constipation, and difficulty with bowel movements. The weakened abdominal wall cannot provide adequate support for internal organs, potentially affecting their normal function. Hernias are another serious complication, where internal organs or tissues protrude through the weakened abdominal wall.
Risk factors for developing complications include:
- Delayed treatment or diagnosis
- Multiple pregnancies
- Advanced age at onset
- Obesity or significant weight fluctuations
- Participation in high-impact activities
- Underlying connective tissue disorders
Psychological complications shouldn’t be overlooked either. Many people with visible gastroshiza experience decreased self-esteem, body image issues, and social anxiety. These psychological effects can significantly impact quality of life and may require professional counseling or support groups.
Early intervention and proper treatment can prevent most complications, emphasizing the importance of seeking medical attention when symptoms first appear.
Lifestyle Modifications
Managing gastroshiza successfully often requires making several lifestyle modifications that support healing and prevent further progression. Dietary changes play an important role, particularly focusing on foods that support tissue healing and reduce inflammation. Protein-rich foods help rebuild connective tissue, while foods high in vitamin C and zinc support collagen production.
Avoiding foods that cause bloating or constipation can reduce pressure on the abdominal wall. This includes limiting processed foods, excessive fiber intake, and foods that commonly cause gas. Staying well-hydrated helps maintain healthy tissue elasticity and supports overall digestive health.
Sleep position modifications may be necessary, particularly for those experiencing back pain. Sleeping with a pillow between the knees or using a pregnancy pillow can provide better spinal alignment and reduce strain on the core muscles. Some people find that sleeping slightly elevated helps reduce nighttime symptoms.
Daily activity modifications include:
- Using proper body mechanics when lifting or carrying objects
- Taking frequent breaks during prolonged sitting or standing
- Wearing supportive clothing or compression garments
- Avoiding activities that cause visible bulging or discomfort
- Practicing stress management techniques to reduce overall tension
These lifestyle changes, when combined with appropriate medical treatment, can significantly improve outcomes and prevent complications.
When to See a Doctor
Knowing when to seek professional medical help for gastroshiza is crucial for preventing complications and achieving the best possible outcomes. You should consult a healthcare provider if you notice a visible bulge or gap in your abdominal muscles, especially if it’s accompanied by pain, discomfort, or functional limitations.
Immediate medical attention is warranted if you experience severe abdominal pain, nausea, vomiting, or signs of a hernia (a hard lump that doesn’t reduce when lying down). These symptoms could indicate serious complications that require urgent treatment.
You should also see a doctor if conservative treatments haven’t shown improvement after 2-3 months of consistent effort, or if the condition is significantly impacting your daily activities or quality of life. Healthcare providers can offer additional treatment options and determine if surgical intervention might be beneficial.
Regular follow-up appointments are important for monitoring progress and adjusting treatment plans as needed. Your doctor can assess whether your current approach is working and make recommendations for modifications if necessary. Don’t hesitate to ask questions or express concerns during these visits – open communication with your healthcare team is essential for successful treatment.
As highlighted in recent medical discussions on TrendsMag, early medical intervention has been shown to improve long-term outcomes significantly, making prompt professional consultation highly recommended.
Long-term Outlook and Recovery
The long-term outlook for people with gastroshiza is generally positive, especially when the condition is diagnosed early and treated appropriately. Most cases respond well to conservative treatment, with significant improvement seen within 6-12 months of consistent therapy. Complete healing is possible in many cases, particularly for mild to moderate separations.
Recovery time varies depending on several factors, including the severity of the separation, individual healing capacity, compliance with treatment recommendations, and overall health status. Younger patients typically heal faster than older individuals, and those who maintain good overall fitness during treatment tend to have better outcomes.
For cases requiring surgical intervention, the success rate is high, with most patients experiencing significant improvement in both function and appearance. However, surgery does carry risks and requires a longer recovery period, typically 6-8 weeks for initial healing and several months for complete recovery.
Long-term management may include:
- Ongoing exercise programs to maintain core strength
- Regular monitoring for recurrence
- Lifestyle modifications to prevent re-injury
- Periodic reassessment by healthcare providers
The key to successful long-term outcomes is understanding that gastroshiza management is often an ongoing process rather than a one-time treatment, requiring continued attention to core health and proper body mechanics.
Key Takeaways
Understanding gastroshiza is essential for anyone experiencing symptoms or at risk for developing this condition. This digestive and abdominal muscle disorder affects millions of people worldwide but can be effectively managed with proper diagnosis and treatment. Early recognition of symptoms, including visible muscle separation and associated discomfort, leads to better treatment outcomes.
Conservative treatment approaches, including specialized exercise programs and physical therapy, are often successful for mild to moderate cases. Severe cases may require surgical intervention, but the overall prognosis remains positive with appropriate care. Prevention strategies, including maintaining core strength and using proper body mechanics, can help reduce the risk of developing gastroshiza.
Lifestyle modifications play a crucial role in both treatment and prevention, emphasizing the importance of a holistic approach to managing this condition. Regular medical monitoring ensures optimal outcomes and helps prevent complications that could impact long-term health and quality of life.
Conclusion
Gastroshiza is a manageable condition that doesn’t have to significantly impact your quality of life when properly addressed. By understanding the causes, recognizing symptoms early, and working with healthcare professionals to develop an appropriate treatment plan, most people can achieve significant improvement or complete recovery.
Remember that healing takes time, and consistency with treatment recommendations is crucial for success. Whether your treatment involves exercise therapy, lifestyle modifications, or surgical intervention, maintaining realistic expectations and staying committed to your recovery plan will give you the best chance of achieving your goals.
If you suspect you might have gastroshiza or are experiencing related symptoms, don’t hesitate to seek professional medical advice. Early intervention is key to preventing complications and achieving the best possible outcomes. With proper care and management, you can regain core strength, reduce symptoms, and return to your normal activities with confidence.
Frequently Asked Questions
Q: Is gastroshiza the same as diastasis recti?
A: While the terms are sometimes used interchangeably, gastroshiza specifically refers to the splitting or separation of stomach muscles, whereas diastasis recti is the medical term for abdominal muscle separation. They describe essentially the same condition.
Q: Can gastroshiza heal on its own without treatment?
A: Mild cases may improve naturally over time, especially postpartum gastroshiza. However, most cases benefit significantly from targeted treatment, and severe cases typically require intervention to prevent complications.
Q: How long does it take to see improvement with exercise therapy?
A: Most people begin to see improvement within 6-8 weeks of consistent, proper exercise therapy. Complete healing may take 6-12 months or longer, depending on the severity of the condition.
Q: Can men develop gastroshiza?
A: Yes, while less common than in women, men can develop gastroshiza due to factors like heavy lifting, rapid weight gain, or genetic predisposition to weak connective tissue.
Q: Will gastroshiza return after successful treatment?
A: Recurrence is possible if risk factors aren’t managed properly. Maintaining core strength, using proper body mechanics, and avoiding excessive abdominal pressure help prevent recurrence.
Q: Is surgery always necessary for severe gastroshiza?
A: Not always. Some severe cases respond to intensive conservative treatment, though surgery may be recommended when other treatments haven’t been successful or when complications are present.